ID and IDA Impact Millions of People Who Deserve a Treatment That Makes Them Feel Better, Not Worse1
Iron Deficiency and Iron Deficiency Anemia Are Serious, Prevalent, and Often Undertreated1
Iron Deficiency vs Iron Deficiency Anemia
The medical terms iron deficiency (ID) and iron deficiency anemia (IDA) are sometimes used interchangeably. However, ID can occur with or without the presence of anemia.2
- Absolute ID2
- The reduction of total body iron stores, which can progress in severity, leading to IDA
- Occurs mostly in macrophages and hepatocytes
- Functional ID2
- Iron is not effectively mobilized from stores to circulation
- Insufficient stored iron results from increased erythropoiesis by endogenous erythropoietin or by erythropoiesis-stimulating agents
- IDA is defined as hemoglobin levels <13 g/dL (men), <12 g/dL (nonpregnant women), and <11 g/dL (pregnant women) and serum ferritin <30 mcg/L OR serum ferritin <100 mcg/L in the presence of inflammation2
- IDA can be due to a wide range of different causes, which can be grouped into three major categories: iron imbalance, blood loss (occult or overt), and malabsorption1
- In the United States approximately 10 million people have ID and 5 million have IDA1
ID and IDA prevalence are high in patients with inflammatory conditions or in women of childbearing age

ID: 50-72%
IDA: 17-44%

ID: 20-65%
IDA: 11-27%

ID: 36-90%
IDA: 36-76%

ID: 33-50%
IDA: ~66%

ID: 20-65%
IDA: 7-42%
Prevalence estimates differ due to the disease stage and severity of the patient population being studied.
CKD, chronic kidney disease.
IBD, inflammatory bowel disease.
~20% of women of childbearing age and up to 37% of pregnant women may have IDA9,10
The Complexities of Treating ID
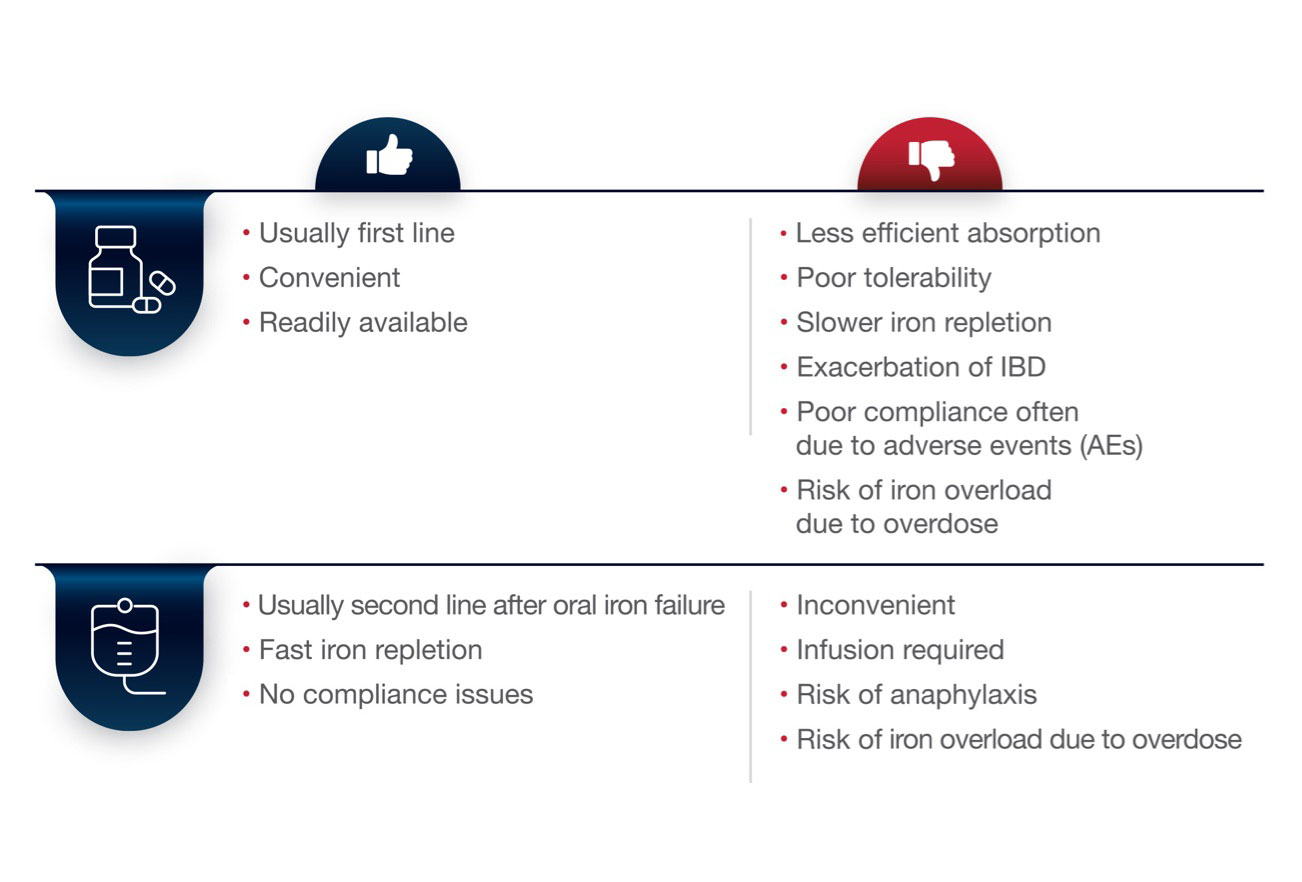
A comparison of traditional iron salts and IV iron2,11
- Many IDA patients have an underlying condition that makes them susceptible or severely symptomatic to COVID-1912
- Recommendations for caring for at-risk patients include consideration of home treatments and switching patients from IV to oral therapies to minimize exposure13
Current Oral Iron Salts Have Been Associated With High Rates of AEs
- Oral iron replacement therapies are typically used first line to treat IDA but have poor gut tolerability, inefficient absorption and efficacy, and poor patient adherence14,15
- Up to 70% of people taking oral iron report gastrointestinal (GI) issues, which can affect therapy adherence14
- Nonadherence to therapy can lead to substantial treatment failures and additional unwarranted follow-up studies15
- IV iron should be considered when there is intolerance/poor response to oral iron therapy, a need to raise iron levels rapidly, before or after surgery, or with certain medical conditions such as CKD with dialysis, Class II-IV chronic heart disease, and in certain cases in the second and third trimesters of pregnancy2
AEs and gastrointestinal (GI) AEs may lead to nonadherence in nearly half of IDA patients
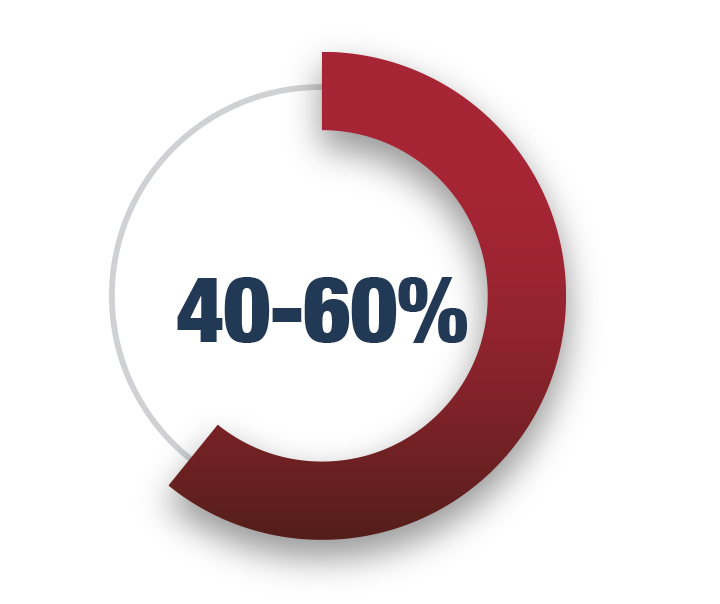
Estimated overall adherence with oral iron for IDA due to all AEs16
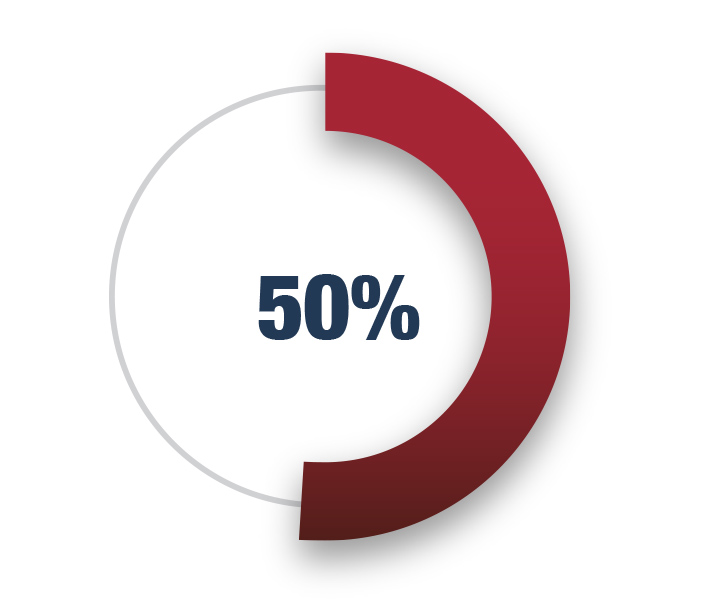
Estimated overall adherence with oral iron for IDA due to GI AEs15
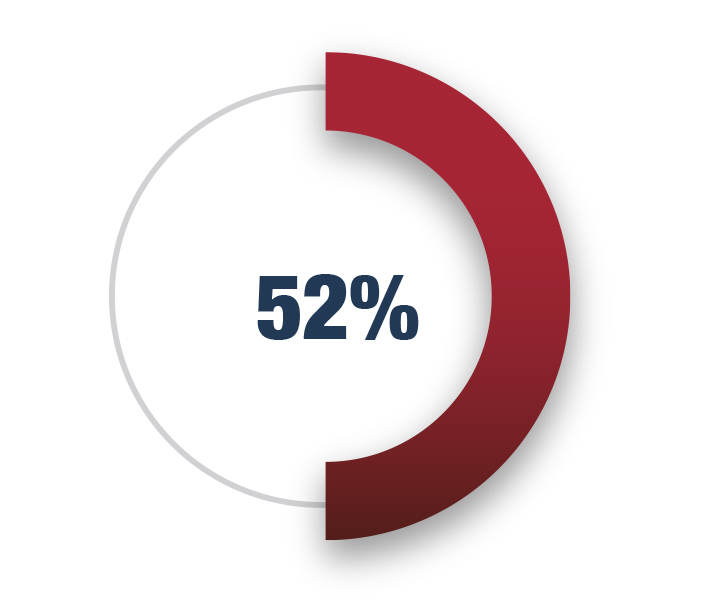
Of IBD patients with IDA reduce or withdraw oral iron dose due to AEs17
IV iron should be considered when there is intolerance/poor response to oral iron therapy, a need to raise iron levels rapidly, before or after surgery, or with certain medical conditions such as CKD with dialysis, Class II-IV chronic heart disease, and during pregnancy2
Discover How ACCRUFeR® (ferric maltol) Is Unique
References
1. Miller JL. Iron deficiency anemia: a common and curable disease. Cold Spring Harb Perspect Med. 2013;3:a011866. 2. Cappellini MD, Musallam KM, Taheret AT. Iron deficiency anaemia revisited. J Intern Med. 2020;287(2):153-170. 3. Klip IT, Comin-Colet J, Voorset AA, et al. Iron deficiency in chronic heart failure: an international pooled analysis. Am Heart J. 2013;165(4):575-582.e573. 4. Cohen-Solal A, Damy T, Terbah M, et al. High prevalence of iron deficiency in patients with acute decompensated heart failure. Eur J Heart Fail. 2014;16(9):984-991. 5. Fishbane S, Pollack S, Feldman HI, Joffeet MM, et al. Iron indices in chronic kidney disease in the national health and nutritional examination survey 1988–2004. Clin J Amer Soc Neph. 2009;4(1):57-61. 6. Stein J, Hartmann F, Dignass AU. Diagnosis and management of iron deficiency anemia in patients with IBD. Nat Rev Gastroenterol Hepatol. 2010;7(11):599-610. 7. Kulnigg S, Gashe C. Systematic review: managing anaemia in Crohn’s disease. Aliment Pharm & Ther. 2006;24(11-12):1507-1523. 8. Naoum FA. Iron deficiency in cancer patients. Rev Bras Hematol Hemoter. 2016;38(4):325-330. 9. Friedman AJ, Chen Z, Ford P, et al. Iron deficiency anemia in women across life span. J Womens Health (Larchmt). 2012;21(12):1282-1289. 10. Your Guide to Anemia. National Heart, Lung, and Blood Institute website. https://www.nhlbi.nih.gov/files/ docs/public/blood/anemia-yg.pdf. September, 2011. 11. Jimenez K, Kulnigg-Dabsch S, Gasche C. Management of iron deficiency anemia. Gastroenterol Hepatol (N Y). 2015:;11(4): 241-250. 12. Hariyanto TI, Kurniawan A. Letter to the editor: anemia is associated with severe coronavirus disease 2019 (COVID-19) infection. Transfus Apher Sci. 2021.p1-3. [article in press]. 13. InCrowd Novel Coronavirus (COVID-19) Patient Tracking Report, wave 1, April 2, 2020 14. DeLoughery TG: Safety of oral and intravenous iron. Acta Haematol. 2019;142:8-12. doi: 10.1159/000496966. 15. Tolkien Z, Stecher L, Mander AP, Pereira DIA, Powell JJ. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS ONE. 2015;10(2); e117383. doi:10.1371/journal.pone.0117383. 16. Cancelo-Hidalgo MJ, et al. Tolerability of different oral iron supplements: a systematic review. Curr Med Res Opin. 2013;29(4):291-303. 17. Lindgren S, Wikman O, Befritset R, et al. Intravenous iron sucrose is superior to oral iron sulphate for correcting anaemia and restoring iron stores in IBD patients: a randomized, controlled, evaluator-blind, multicentre study. Scand J Gastroenterol. 2009;44(7):838-845.
